Oct 30, 2025
TennCare: Tennessee’s Medicaid Transformation Story
From Crisis to Cornerstone: How Tennessee Rebuilt Its Healthcare Safety Net
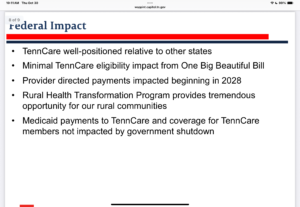
I’m sitting in the Tennessee House, Finance, Ways and Means Committee listening the a presentation by Tenncare Commissioner Steve Smith. The issue of Tenncare and Medicare is very complicated. I thought I’d share some information and add the presentation for those who care about this issue.
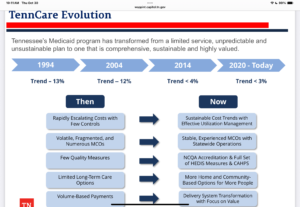
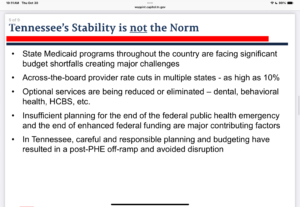
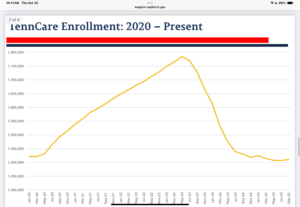
The landscape of American healthcare, few states have experienced as dramatic a transformation in their Medicaid programs as Tennessee. TennCare, the state’s managed care Medicaid program, has evolved from a bold but troubled experiment in the 1990s to become a stable, comprehensive system that serves as a lifeline for more than 1.6 million Tennesseans.

The Ambitious Beginning
TennCare launched in 1994 with revolutionary ambitions. Governor Ned McWherter’s administration sought to solve two critical problems simultaneously: control escalating Medicaid costs and expand coverage to Tennessee’s uninsured population. The program replaced traditional fee-for-service Medicaid with a managed care model, contracting with private health plans to deliver services.
The initial vision was sweeping. TennCare would not only cover traditional Medicaid-eligible populations but also extend coverage to the “uninsurable”—people with pre-existing conditions who couldn’t obtain private insurance—and the “uninsured”—working Tennesseans who earned too much for Medicaid but couldn’t afford private coverage.
At its peak in the early 2000s, TennCare covered approximately 1.4 million people, including nearly 500,000 who would not have qualified under traditional Medicaid rules.















Leave feedback about this